-6 Stem Cell & Types of Stem Cells?
페이지 정보

본문
1. Stem cells?
In English, it is stem cell. Stem is a stem cell, so it is a stem cell. There are many words that mean the meaning of stem in English, and among them, stem corresponds to the main stem, and branches spread out in all directions from the stem. So stem means origin, and stem cell means a cell before differentiation into various cells.
2. when and how are stem cells discovered?

It is complicated to explain in words, so I will briefly explain it while looking at the history. The first stem cells were discovered in bone marrow in 1963. Bone marrow exists within the bones that make up our bodies, and when we collected this bone marrow and studied it, we found that stem cells that differentiate into various blood cells exist. The discovery of bone marrow stem cells opens the way to curing leukemia patients in the future. In other words, the leukemia patient's bone marrow is removed and healthy bone marrow is transplanted to treat leukemia.
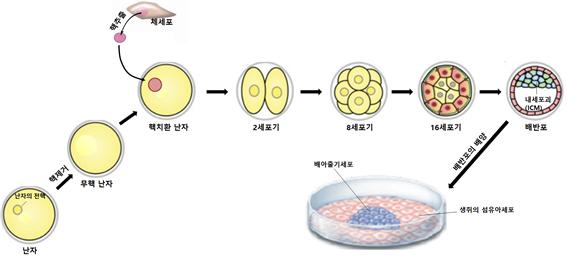
Later, through independent studies, embryonic stem cells were discovered in mice in 1981, and neural stem cells in the brain were discovered for the first time in organs other than bone marrow in 1992. In 2001, it became possible to produce customized mouse embryonic stem cells using nuclear transfer technology, and in 2006, a method was developed to easily produce human induced pluripotent stem cells.
3. In the previous explanation, you used terms such as embryonic stem cells, bone marrow stem cells, and induced pluripotent stem cells. What do these terms mean?
Although we usually refer to them collectively as stem cells, there are various types of stem cells. Stem cells can be broadly divided into embryonic stem cells and adult stem cells. In addition, there is something called induced pluripotent stem cell (iPS cell). Bone marrow stem cells and neural stem cells are types of adult stem cells. Embryonic stem cells have the ability to differentiate into all cells that make up a person, while adult stem cells have the ability to differentiate into limited cells. You can think of induced pluripotent stem cells as having almost similar abilities to embryonic stem cells.
4. So what are induced pluripotent stem cells(IPS)?
The stem cells that replace customized embryonic stem cells are induced pluripotent stem cells. Professor Yamanaka's team in Japan was the first to produce induced pluripotent stem cells. When four genes (c-Myc, Oct4, Sox2, Klf4) are simultaneously expressed in fibroblasts obtained from the skin of a patient in need of customized embryonic stem cells, the fibroblasts become cells similar to embryonic stem cells, and these cells are called induced pluripotent stem cells. They are called cells.
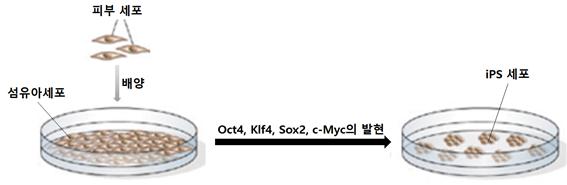
Professor Yamanaka's team's method has the advantage of low technical difficulty and a 100% success rate because it does not go through a nuclear substitution process.
5. please tell us about adult stem cells.
Almost all tissues in humans contain stem cells to repair damage to the tissue. For example, there are bone marrow stem cells that exist in the bone marrow, muscle stem cells that exist in the muscles, vascular stem cells that exist in the venous blood, neural stem cells that exist in the brain, and adipose stem cells that exist in the fat. These stem cells are collectively called adult stem cells.
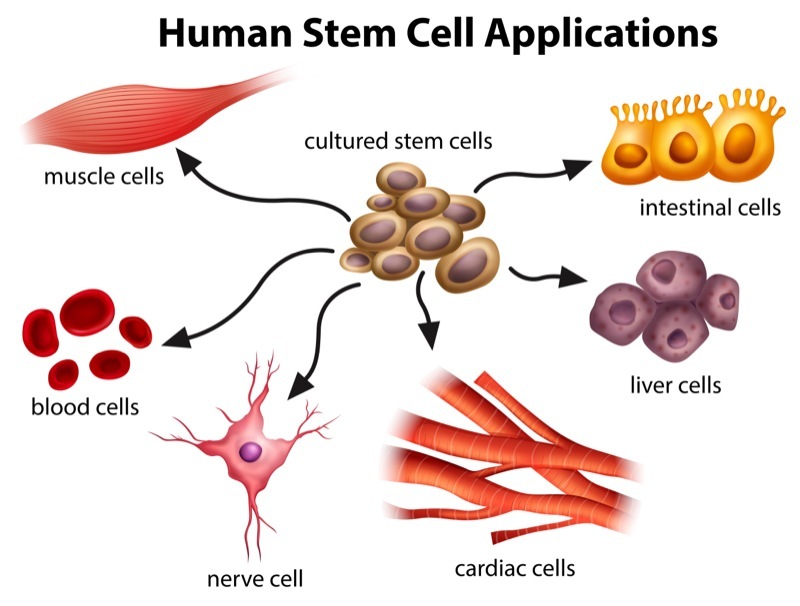
The reason adult stem cells are stem cells is because these cells have the ability to differentiate into various types of cells. For example, fat-derived stem cells can differentiate into bone cells, cartilage cells, nerve cells, etc. in addition to fat cells. Unlike embryonic stem cells, adult stem cells are limited in the types of cells that can be differentiated. The reason for this limitation in differentiation is that adult stem cells are already highly differentiated cells with a limited fate. This may be a disadvantage, but it is a great advantage in terms of safety. Adult stem cells are already highly differentiated cells, so unlike embryonic stem cells, there is little chance of developing cancer when transplanted. Therefore, unlike embryonic stem cells, they are actively used clinically. In particular, adipose stem cells have the advantage of being relatively large in quantity and easy to collect, so it is no exaggeration to say that almost all current adult stem cell research uses adipose stem cells.
2-1. Stem cells and fat
1. What is fat?
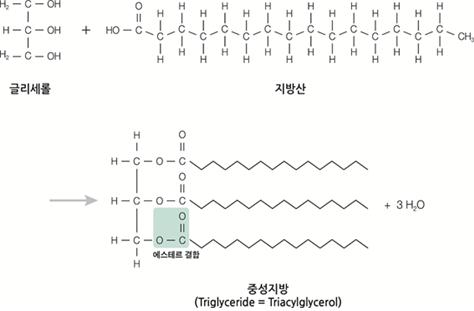
Biologically, fat refers to a triacylglyceride consisting of one glycerol molecule and three fatty acid molecules in an ester bond.
However, the fat we commonly refer to means adipose tissue. In other words, when you say, “I have too much fat in my body,” the fat is adipose tissue. So, this video is about fatty tissue.
2. Are all fatty tissues the same?
It's not like that. Adipose tissue can be divided into white fat and brown fat depending on its characteristics. White fat is composed of cells for the purpose of storing fat, and when energy sources are depleted, it breaks down its own fat and supplies fatty acids as an energy source to other tissue cells. So, it usually contains huge fat droplets and has a small number of mitochondria, so it is yellow in color. On the other hand, brown fat, which has a brown color because it contains a large amount of mitochondria in the cells, exists to produce heat by oxidizing its own fat. Therefore, it is relatively small compared to white fat and contains a heat-producing protein called thermogenin in its mitochondria.
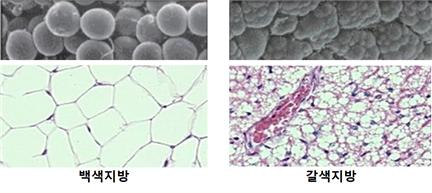
Brown fat accounts for approximately 5% of body weight in infancy, but is only slightly present in adulthood, mainly in the shoulders and chest. There is an old saying, ‘No matter how cold it is, babies and crock pots do not freeze.’ It seems that our ancestors were empirically aware of the existence of brown fat in newborns.
3. How is adipose tissue composed?
As mentioned earlier, adults have very little brown fat, so we will only look at white fat. Adipose tissue is composed of fat cells, extracellular matrix, and blood vessels. The extracellular matrix is again composed of connective fibers such as collagen and various cells. Adipose stem cells (ADSC), pericytes, macrophages, lymphocytes, and fibroblasts are cells that exist in the extracellular matrix.
SVF (stromal vascular fraction), which is attracting attention these days, can be thought of as the sum of cells present in the extracellular matrix and blood vessels of adipose tissue. The adipocytes that make up adipose tissue are spherical cells with a diameter of about 70 to 140 μm and, when mature, contain huge fat droplets in their cytoplasm. Adipose tissue has a dense capillary network and consumes little oxygen due to its low energy consumption rate, thus maintaining the highest partial
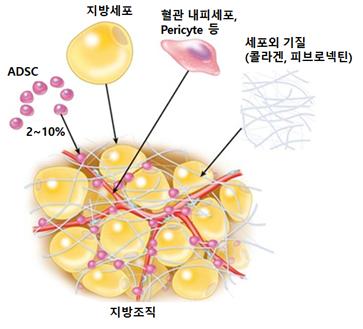
pressure of oxygen among tissues in the body.
4. So what are subcutaneous fat and visceral fat?
Fat tissue is classified according to location.
Subcutaneous fat is located just beneath the skin and directly above the muscles. Subcutaneous fat can be felt when touching the skin, and is present all over the body, but especially in the abdomen, buttocks, and thighs. On the other hand, visceral fat surrounds major organs such as the liver and intestines in the abdominal cavity. Therefore, you cannot feel the presence of visceral fat with your hands.

5. Is there any difference between subcutaneous fat and visceral fat?
There is a big difference in two ways.
First of all, the causes of the formation of the two fats are different. Subcutaneous fat is mainly accumulated when excessive consumption of high-fat foods occurs. On the other hand, drinking alcohol is the main cause of visceral fat accumulation. The two provinces have different roles. Small amounts of subcutaneous fat promote health. Not only does it provide energy when needed, it produces hormones such as leptin to make you feel full, and produces adiponectin to help maintain healthy blood sugar levels. On the other hand, visceral fat is harmful to health. Excessive visceral fat can cause heart disease, high blood pressure, diabetes, stroke, and colon cancer, so be careful. Since 44% of women and 42% of men have excessive visceral fat, the risk factor may be greater than you think.
2-2. Intravenous stem cells?
1. What are intravenous stem cells? Worldwide, SVF and ADSC are used for intravenous administration. As we have already explained the difference between SVF and ADSC several times in several previous videos, SVF is the cells of the stroma and blood vessels contained in adipose tissue, and ADSC refers only to adipose stem cells proliferated after culturing SVF. However, our country's medical law practically prohibits the use of cultured ADSC cells, so our hospital administers SVF intravenously.
2. Please briefly explain how to inject SVF intravenously. As mentioned in the previous video, SVF is obtained after processing extracted fat tissue with an enzyme called collagenase. SVF is composed of various cells and fibrous proteins, and among these, ADSC are the ones that play the main role after intravenous injection of SVF. In adipose tissue, ADSCs exist in a resting G0 state with cell division suspended. To wake these cells up to divide, platelets from the blood, or PRP, are mixed. SVF contains clumps of fibrous proteins such as collagen. These fibrous proteins are large and can block blood vessels and impede blood flow. Therefore, the mixture of PRP and SVF must be filtered through a type of sieve called a cell strainer before being injected into a vein. The filtered cell suspension can now be injected into the patient's vein.

3. Are there any additional considerations when injecting SVF?
The amount of SVF used per injection is important. It can be easily expected that if too small an amount of SVF is injected intravenously, the effect will be minimal, right? The amount of SVF injected increases in proportion to body weight, and usually more than 1 million cells per kg must be injected to be effective. For example, this means that a person weighing 70 kg would need to be injected with approximately 70 million cells. The more frequent injections, the better, but it is known that the effect usually appears in one injection and takes up to one month.
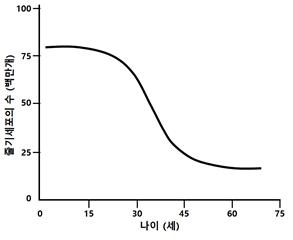
4. What are the benefits of intravenous stem cell injection? It is known to have anti-aging and disease-curing effects. According to research results to date, one of the important reasons why people age is that the number of stem cells decreases with age. Each human tissue contains adult stem cells. When each tissue is damaged, these adult stem cells play a role in healing the damage by dividing and differentiating on their own. However, as a person ages, the number of adult stem cells decreases, their activity decreases, and their ability to repair tissue damage decreases, leading to aging. This fact can be seen through our experience. Wounds suffered when we are young are easily healed and rarely leave scars, but as we age, the healing period for the wounds takes longer and severe scars remain. Additionally, as you age, your skin becomes thinner. If the decline in stem cells is the main cause of aging, then aging can be prevented or overcome by maintaining the number and activity of stem cells. In other words, if ADSCs, adult stem cells present in SVF, are consistently supplied intravenously, it can be expected to have an anti-aging effect. In fact, the following anti-aging effects were observed in patients who received SVF intravenous injection. The elasticity and tone of the skin, especially the face and hands, has improved, arthritic pain and joint weakness have disappeared or been significantly reduced, muscle pain has disappeared or been significantly reduced, energy and ability to perform daily tasks have increased, and memory has improved. This improved, and my vision and hearing improved somewhat. Urinary incontinence and ability to defecate have improved. Currently, there is a limitation in that continuous SVF intravenous injections cannot be administered due to the cost burden, but if this procedure becomes popular in the future, it is expected that it will contribute to maintaining our youth. Regarding disease healing, SVF has immunomodulatory ability, angiogenesis ability, and growth factor secretion ability. Among these, the immunomodulatory ability shows a therapeutic effect on inflammatory reactions or autoimmune diseases such as atopy, severe psoriasis, allergic rhinitis, asthma, multiple sclerosis, emphysema, alopecia areata, and pneumonia caused by COVID19. Abilities such as immunomodulatory ability and secretion of growth factors appear to improve brain-related diseases, improving symptoms in patients with Parkinson's disease, insomnia, migraine, autism, stroke, and traumatic brain injury. In addition to these diseases, it is also known to play a role in improving the symptoms of diabetes and erectile dysfunction.
5. Are there any side effects from intravenous stem cell injection? The safety of SVF injection can be found out through the results of the paper published by Comella et al. (Comella et al., J Clin Med Res. 2017;9(11):935-942). Comella et al. collected data from five medical institutions in the United States and then analyzed this data. Each medical institution injected SVF using various methods into a total of 676 different patients. As a result of investigating the safety of SVF in various patients who received SVF injection through various routes, in most cases, more than 90% of patients showed no side effects. The only side effects that appeared were swelling and fever, and a complete recovery was possible with simple drug treatment. These research results clearly demonstrate that SVF surgery is safe.
6. What are the directions for the development of intravenous stem cell injection? We will answer this question with recent research trends. Among the properties of ADSC, there is something called the homing effect. ADSC injected intravenously travels to the patient's uncomfortable or diseased areas and provides treatment. However, actual research has shown that ADSCs injected intravenously travel to the lungs, liver, and brain, where they accumulate the most and then disappear. In other words, the homing effect is not as clear as you might think. Therefore, current researchers are studying methods that can force ADSCs to home to a desired area. As these studies accumulate, we can look forward to customized stem cell treatments.
2-3. How long do the effects of stem cells last?
It is difficult to give an exact answer as the duration of the effects of stem cells varies depending on the disease, treatment method, and individual patient condition. But in general, it tends to be something like this:
1. Disease Neurological diseases: For Parkinson's disease, Alzheimer's disease, etc., the effects of stem cell therapy may last for several years, but may not completely prevent disease progression. Cardiovascular disease: In cases such as myocardial infarction and heart failure, the effects of stem cell therapy can last for several years and can help improve heart function and improve survival rates. Blood diseases: For leukemia, anemia, etc., stem cell treatment can lead to cure, but there is a possibility of recurrence. Immune disorders: For conditions such as diabetes and rheumatoid arthritis, stem cell therapy may help relieve symptoms, but may require ongoing treatment. Tissue damage: For burns, fractures, etc., stem cell therapy may help with tissue regeneration, but rehabilitation is required and full recovery may take a long time.
2. Treatment method Stem cell type: The duration of effect may vary depending on the type of stem cell, such as embryonic stem cells, adult stem cells, and iPS cells. Caution must be exercised with embryonic stem cells or IPS as they have a risk of tumor formation, and MSCs do not form tumors, but their therapeutic effectiveness is somewhat lower. Therefore, we are focusing on Wharton Jelly stem cell treatment, which has no tumor risk and higher efficacy than IPS. Method of administration: The duration of effect may vary depending on the method of administration, such as intravenous injection, local injection, or direct implantation. Number of doses: The duration of effect may vary depending on single or repeated doses.
3. Patient’s individual condition Age: The older you are, the less likely the effects of stem cell treatment will last. Health status: The better your health, the longer the effects of stem cell treatment may last. Immune system: When using blood-derived stem cells, a stronger immune system may increase the likelihood of stem cell rejection, which may shorten the duration of effectiveness. Therefore, if you are considering stem cell treatment, it is important to consult with a medical professional to obtain accurate information tailored to your disease, treatment method, and individual condition.
2-4.Are stem cells frozen?

Yes, it is better to freeze-dry stem cells rather than freeze them for storage purposes. Reasons for freeze-drying stem cells:
Long-term storage: Stem cells can remain active for a long period of time through freeze-drying.
Prevents cell damage: Freeze-drying helps maintain stem cell function by preventing cell damage.
Easy to transport and distribute: Freeze-dried stem cells are easy to transport and distribute, making them easy to get to where they are needed.
Stem cell freeze-drying:
Liquid nitrogen storage: Frozen stem cells are stored at a temperature of liquid nitrogen (-196°C).
Advantages of stem cell freezing:
Can be stored for a long time
Prevent cell damage
Easy to transport and distribute
Disadvantages of stem cell freezing:
Possibility of cell damage during freezing process
Requires skilled skills and equipment
Storage costs incurred
Precautions regarding stem cell freezing:
Frozen stem cells require the use of skilled techniques and equipment as there is a risk of cell damage during the thawing process.
Conclusion: Stem cells are often frozen for long-term storage, to prevent cell damage, and for ease of transportation and distribution. However, there is a possibility of cell damage during the freezing process and skilled techniques and equipment are required.
Therefore, freeze-drying rather than freezing is superior for storage and transportation.
- PrevWhat is the biggest advantage of Panacell Biotech as a research institution? 24.04.15
- NextWhat are mesenchymal stem cells (MSC) 24.04.16
댓글목록
등록된 댓글이 없습니다.





 +82-2-593-3210
+82-2-593-3210 info@panacellbio.com
info@panacellbio.com 3F, Inspire Ent. Resort, 127 Jung-gu, Incheon, Republic of Korea
3F, Inspire Ent. Resort, 127 Jung-gu, Incheon, Republic of Korea